In an age of increasing data breaches, keeping patients’ medical information secure becomes critical for health care providers. In 1996, the Centers for Disease Control and Prevention created HIPAA (Health Insurance Portability and Accountability Act of 1996) to protect sensitive patient information from becoming compromised without the patient’s consent or knowledge.
In other words, health care providers must proactively work to make sure patient information is secure from cyberattacks.
Hospitals and clinics that work with protected health information (PHI) must have the physical, process and network security protocols set up to ensure HIPAA compliance. All careers in health care are subject to HIPAA compliance measures.
According to a study by CyberMDX, 80% of device manufacturers and health care organizations concluded that medical devices are challenging to secure. Moreover, 53% of health care delivery organizations say that there is a lack of quality assurance and testing that leads to a potentially compromised system.
Altogether, the health care industry faces severe challenges in combating cybersecurity threats.
In this article, we will look at the following:
- Cybersecurity Risks in Health Care
- HIPAA Security and Privacy Rules
- Is HIPAA Compliance Enough?
- Ways to Maintain HIPAA Compliance and Cybersecurity
Cybersecurity Risks in Health Care
In September of 2020, there were over 9.7 million records compromised. This was a 156.75% increase compared to August 2020. Hackers are the main culprits of data breaches.
Consequently, a lot of health care providers have begun using artificial intelligence as a means to thwart hackers and threats to cybersecurity. AI can identify new malware threats by using predictive algorithms (computer instructions geared toward solving a problem), detecting and responding to breaches, and addressing smart medical devices’ security challenges.
However, AI is not perfect. For example, the artificial intelligence company Cense AI accidentally leaked the data of over 2.5 million patients in 2020. Also, cybercriminals have discovered ways to trick AI systems.
The growth of remote medicine has increased the risks for cyber attacks as well. For example, many patients use wearable sensors that monitor patient health statistics and remote care measures like these increase cyber attacks’ potential.
It’s critical for health care providers to take extra measures to prevent these invasions.
For instance, leveraging risk assessment services can help identify vulnerabilities in their systems and implement stronger cybersecurity protocols. Additionally, encrypting patient data, using multi-factor authentication, and regularly updating software can further protect sensitive information from cyber threats.
That said, some of the most common cybersecurity risks that hospitals and health care clinics face are:
Phishing Attacks:
A phishing attack attempts to gain sensitive information by pretending to be a credible entity within digital communication. For health care providers, this can come in the form of an email that seems to be from a company or service that the employees deal with regularly.
Malware:
It is software designed to disrupt a computer network. These come in the form of viruses, worms and Trojan horses, among other things.
Cloud Threats:
More companies move their data into cloud programs that allow providers to access software exclusively on the internet. Moving the data to cloud-based platforms puts providers at risk since hackers can access it remotely.
HIPAA Security and Privacy Rules
The HIPAA Privacy Rule protects all “individually identifiable health information” possessed or transferred by a covered entity or its business affiliate in any form of media.
Cybersecurity is explicitly covered by the Security Rule that falls under HIPAA’s Title ⅠⅠ. The rule declares that providers must establish and maintain protections for electronic PHI that defends the organization against breach through physical, administrative and technical means.
The rule states that HIPAA-compliant organizations must:
- Ensure that all health data they send, store, receive or produce has vital availability, integrity and confidentiality. (Availability indicates that authorized individuals can access and use their information whenever they want. Integrity means that only accepted means should be used for the destruction or changing of health data. Confidentiality denotes that it is only made available to and is only disclosed to authorized people.)
- Detect and safeguard against any foreseen threats to the data’s integrity or security.
- Defend against any disclosure or use that unauthorized by HIPAA
- Verify that the workforce is compliant with health care law.
These stipulations are effective ways to combat cybersecurity attacks. They create systems to mitigate disclosing PHI. Moreover, the Security Rule requires risk analysis as a central part of the security management process.
The covered entity must review its records to track access to electronic PHI and find security issues. It must also regularly determine threats to e-PHI.
HIPAA Security and Telehealth
During the COVID-19 pandemic, more and more patients communicate to their clinicians through electronic means or telehealth appointments. According to the U.S. Department of Health & Human Services, HIPAA-covered entities may use remote communication applications such as FaceTime, Facebook Messenger, Google Hangouts, Zoom or Skype.
Clinicians can use these products even if the application does not fully comply with HIPAA rules.
However, clinicians can’t use apps such as Facebook Live, Twitch or TikTok to provide telehealth services.
Is HIPAA Compliance Enough
Unfortunately, HIPAA compliance is not enough to combat all cybersecurity risks. Data breaches happen all the time and will continue happening. Due to the complexity of HIPAA, it takes many resources to thwart cybercriminals.
Many healthcare providers spend their time trying to meet HIPAA standards. At the same time, those protocols might not protect providers from immediate and severe threats.
HIPAA does not provide standards for types of security. For example, there isn’t an encryption protocol or format password format.
Moreover, the HIPAA rules, created in 1996, don’t account for today’s risks such as ransomware, cloud-computing or mobile devices.
In short, HIPAA compliance is not enough.
Ways to Maintain HIPAA Compliance and Cybersecurity
Fortunately, many proactive measures exist to help providers maintain HIPAA compliance and cybersecurity.
Institute a Device Policy
Most health care employees have access to devices like smartphones or tablets throughout their shifts. It’s crucial to employ a device policy for all staff. The last thing you want is a staff member posting sharing PHI on social media or a hacker figuring out an employee’s password and accessing PHI.
The policy can cover everything from secure password policies to device security scanning.
Secure password policies that dictate length, composition and validity periods will help maintain security. Weak passwords provide easier access to potential hackers.
Device security scanning prevents devices from connecting to a health care network without scanning for viruses or malware. This can help keep viruses and malware from going unnoticed and jeopardizing software.
Implement Authorization and Authentication Protocol
Health care providers need to create authentication and authorization protocols to keep their systems safe. These can include two-factor authentication systems, which involve using multiple authentication forms to check an individual’s identity when using a product.
This enables providers security and assurance that their devices are more secure. Also, it makes sure that only authorized users access sensitive material. This boosts cybersecurity as hackers would have to take extra steps to infiltrate a system.
Invest in Security Software
Another essential way to ensure cyber safety involves investing in security software.
Some of the components include firewall, antivirus, encryption and antispyware software.
Firewall:
A firewall is the first defense against malware, viruses and other threats. It monitors and filters incoming and outgoing network traffic. Moreover, it determines whether to allow or block traffic based on security rules.
Antivirus software:
This software is similar to a firewall in that it works to detect malware. However, it goes a step further because it works to prevent and remove malware or viruses.
Encryption:
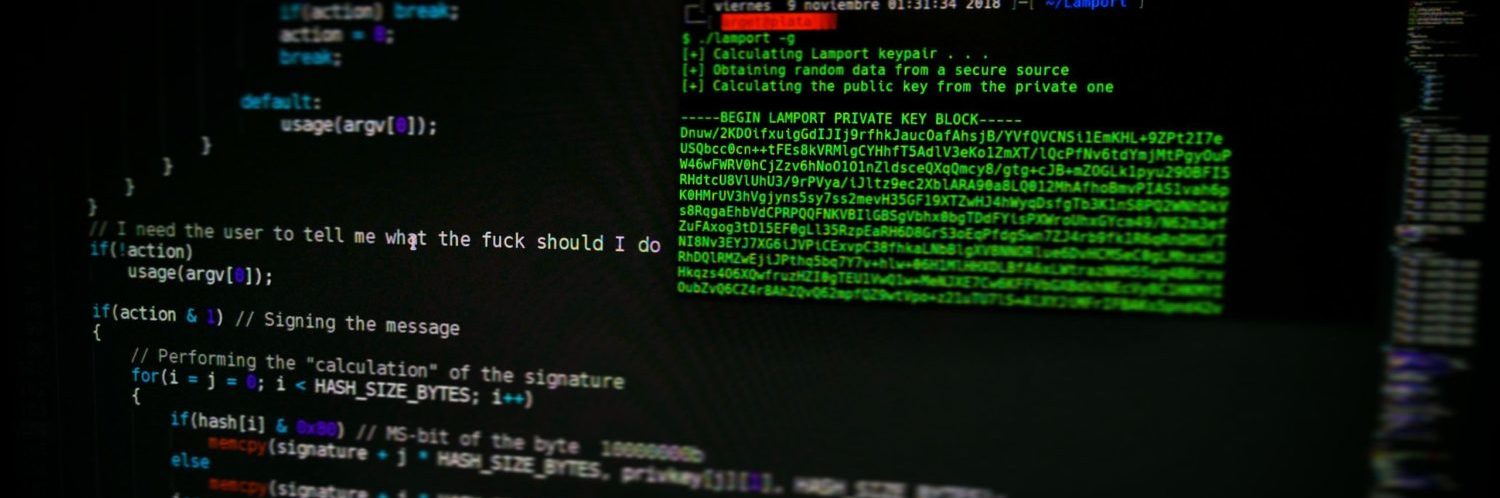
Encryption works by scrambling readable text so that only the person who has the secret code or decryption key can read it. This helps with data security for sensitive information.
Antispyware software:
Antispyware software performs checks on your computer to ensure it is safe and removes unwanted spyware programs. Spyware is a form of malware installed on a computer to collect information.
When combined with HIPAA compliance, all these software programs can help create a secure environment for PHI.
Have a Contingency Plan
Despite the best efforts to avoid data breaches, cybercrime can’t always be prevented. Therefore, it’s critical to have a plan in place in case something does go wrong.
Some of the best ways to plan include: having a backup of important data, creating a response guide to common cyberattacks and assigning an executive to oversee the response plan.
Overall, taking the right steps to secure sensitive patient information can save a company in the long run as the potential fallout of a data breach could cost millions of dollars.
HIPAA compliance is not enough, but providers can achieve a substantial safety degree when combined with the previously mentioned endeavors.